When it comes to effective medicine, information is everything. Genetic testing alone can’t change the realities of DNA, but it can allow the precise reading of DNA, an analysis that spurs preventative measures that save lives. But patients can’t take precautions if they’re never introduced to their own genome.
Testing for the BRCA gene mutation can transform outcomes for women at high risk for breast and ovarian cancer. But Black and Latinx women aren’t getting tested at the same rates as white women. Studies have repeatedly shown that women of color are less likely than white women to be recommended for genetic testing by their doctors, and those who are advised to test meet numerous barriers to entry. Latinx women, especially, face an uphill battle: Breast cancer is the most commonly diagnosed cancer among Latinas in the U.S., yet data from health interview surveys in 2000, 2005, and 2010 showed that Latinas, more than all other U.S. racial ethic groups, had the least awareness about genetic testing. And those who did receive testing couldn’t always act upon what they learned; nearly 20 percent of the U.S. Latina population isn’t covered by health insurance, making preventative surgeries a non-starter.
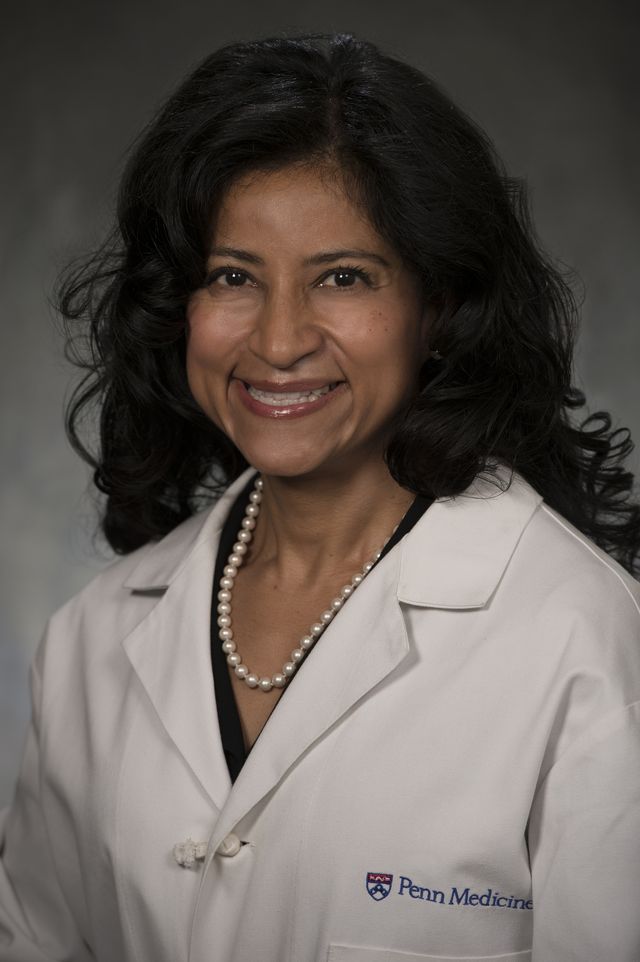
Shifting such a trend in a far-from-perfect healthcare system is a massive challenge, explains Dr. Susan Domchek, director at the Basser Center for BRCA at Penn Medicine, part of the University of Pennsylvania Health System. A medical oncologist who works in genetic testing and cancer management, Domchek is specifically invested in providing access and information to women of color. “We have been really interested in trying to narrow that gap, and that is both by provider education but also patient education,” she says.
Her colleague, Dr. Carmen Guerra, an associate professor of medicine at Penn Medicine who works closely with communities of color, shares the same sentiment. “People of color face many more barriers because of the social determinants of health,” she says. That includes socioeconomic barriers, language barriers, healthcare barriers, and the simple fact that so few doctors—and especially genetic counselors—are people of color themselves. “I try to build programs to address the barriers so that they can access these life-saving cancer screening tests, and be diagnosed at earlier points in time when cancer is the most treatable.”
As Hispanic Heritage Month draws to a close, Domchek and Guerra sat down with ELLE.com to provide a thorough overview of why heritage—the history that composes your genome—is so important to understand, inside and out: It’s not only your story, but a recipe for your health, today and forever. Together, the doctors are working to push this message to communities of color—and Latinas, in particular—so more women can live a life free from cancer.
Why is genetic testing—and especially testing early—so essential?
Domchek: We know that individuals who have mutations in genes, such as BRCA1 and BRCA2, are at very high risk for developing breast cancer and ovarian cancer, particularly. We also know we can do something about these risks. For ovarian cancer risk, our main strategy is removal of the ovaries. For breast cancer, we can offer increased screening by adding breast MRIs onto mammograms, and some women do choose preventative mastectomy. So knowing that you are at risk means you can choose different types of surveillance or prevention options to decrease your chances of developing and dying of cancer.
So why is it that women of color—and in this case, Latinx women—tend to be less likely to undergo this sort of testing?
Guerra: Latinas, especially, face many more barriers, because many of them are more likely to not have insurance. About 20 percent of the Latino population [in the U.S.] actually has no [health] insurance. Furthermore, there are language barriers, and with language barriers comes lack of access to information. And many doctors are not speaking to patients who might be at risk for one of these syndromes sufficiently enough.
One thing we keep seeing in the community over and over again, both in Black women and in Latinx women, is a lack of knowledge of family history. In many communities, as many of my patients have said that it’s taboo to talk about your health in older generations. So people didn’t talk about their cancers, and so they don’t know about their family history.
Finally, I’ll end with the real system barriers. Even if you had a doctor who mentioned this and you have the knowledge [about testing], even if you know your family history and you speak English, you still face barriers like transportation, getting time off work to be able to test and not lose pay, conflicts with family care, elder care, and so forth.
Domchek: We try to chip away at some barriers, but you can only chip away so much. For instance, we have ways we can help cover the cost of genetic testing. But if someone doesn’t have any insurance and we can’t get them a breast MRI, or we can’t refer them to preventative surgery, we didn’t really help them much. Until you have insurance, in the United States it’s really tough.
Guerra: We have a federal law that allows us to provide mammograms for free to women through programs like the one we have at the Abramson Cancer Center. Breast and cervical cancer early detection programs exist all over the country to help women access a mammogram and even a diagnostic work-up, if needed. But, like Susan said, even if we find those women who have breast cancer, and they don’t have insurance, we don’t have any way to cover the surgeries that they need and the treatments that they need. So that’s still a gap in our entire healthcare system. What we have is a series of little patches to address the mammogram need, but then don’t have anything for BRCA screening or for treatment, or for prevention strategies in women who are high-risk.
In what ways do you combat the fear around genetic testing? How do you assure your patients that their genetic information is going to be used safely and ethically?
Domchek: Well, let’s put it bluntly: We’ve given people reasons to mistrust us in the past. And I think regaining that trust is critical. This is why primary care doctors are so important, because most people trust their primary care doctors. They may not necessarily trust the system, but they like their doctor.
Guerra: And not only primary care physicians, but sometimes individuals who are highly trusted in their communities. Because I’ve also seen that same trust be transferred to leaders, especially faith-based leaders. We at the Abramson Cancer Center are fortunate enough to employ a woman who, in her free time, is the volunteer cancer minister at one of the largest [local] churches. We would go to the community with this education about cancer and screening, and they would always turn to our employee and they say, “Well, if Sister Brenda says I should do this, I will do this.” So it isn’t just the doctors, but also there are other influencers in the community that help shape an opinion about medical care. So what we’ve learned to do is partner with them.
Are you seeing change now, in terms of more Latinx women getting tested? How can we achieve progress faster?
Guerra: We are seeing change, but probably not fast enough for Dr. Domchek. [Laughs.] Dispelling [information about] these tests, working with the community and listening to their concerns, working with their trusted messengers—I think it’s been a winning strategy for us. [For example], we’ve been piloting this model where we bring colon cancer screening to the community using a drive-through model with the large churches in Philadelphia. We’ve given out hundreds of FIT kits and helped the Black community identify polyps, so hopefully they won’t [ever] have to hear the words, “You have colon cancer.”
Domchek: I think simplifying who should get testing is really helpful, because then people don’t need to make these complicated decisions. Telemedicine and telegenetics has also been an interesting thing. Our volume for genetic testing went up by 20 percent during the pandemic because we had telegenetics. I’ve had people have appointments with me when they’ve been in their cars during lunch hour. So some of the barriers that Carmen mentioned, we can really get around if we can do [telemedicine].
Let’s say I’m one of your patients. I know my family history, I’ve been informed of why I should undergo testing, I have the time and ability to get tested, and I’ve agreed to do it. What does the process look like next?
Domchek: Ideally, you do have a meeting with a physician or a genetic counselor who reviews your family history to make sure we’re testing for the right genes. And during that assessment with the genetic counselor, the risks and benefits of genetic testing are reviewed. And we do believe there are many benefits in terms of knowing you’re at risk and then taking appropriate measures.
But, for instance, although there is the Genetic Information Nondiscrimination Act, which prohibits the use of genetic information against you for healthcare and your job, it doesn’t prevent your life insurance policy [from going up]. It is important that people know this. [Testing] can certainly be a net benefit, but people need to be aware of what they’re getting when they get this test.
But after going through all of this, you either get your blood drawn or you spit in a tube, and a few weeks later you get your result back. And if that shows something specific, then we launch a plan. And even if it is negative, if you have a strong family history, we often are making different recommendations on screening just on the basis of family history. So genetics isn’t everything; family history still matters. Genetics just add an additional important piece to all of it.
What if, hypothetically, I learn from my genetic test that the likelihood of cancer at some point in my life is high. How do you counsel me through the plan of action? What do you advise as preventative measures?
Domchek: It is complex. Because when we give these risk numbers, for instance, if your lifetime risk of breast cancer is 70 percent, that’s not this year; it’s not next year. It’s over your entire lifetime. So it actually does depend, how old are you? What is your risk over the next five years and 10 years? How important is it for you to breastfeed? Have you found your partner? These are all considerations that really come into play. What is your lived experience of cancer in your family? In some families, there’s been devastation of early deaths from breast cancer. People come in with a different consideration of cancer in those situations.
So it’s our job to take people through it, make them realize that there’s no urgency to decision-making. It’s a series of conversations, and we view ourselves as the quarterbacks that can help people through it. For ovarian cancer, that’s really age-dependent and gene-dependent. So for BRCA1, we’re talking about a preventative removal of the ovaries between 35 and 40. For BRCA2, between 40 and 45. And it’s worth noting that we are working on other strategies besides that; we don’t want to land at only surgical prevention. We view that as what we’ve got now, but we very much hope to have other options for the future.
What are you doing right now to empower the Latinx community to pursue genetic testing? What projects are in the works?
Domchek: Our first approach seemed so simple: We translated our website into Spanish. We made sure that our materials are also available in Spanish. And we’ve tried to expand on our website stories that are being told by Latina women to really be able to, again, give voice to the community.
Guerra: We just established the first cohort of the Abramson Cancer Center Clinical Trials Ambassadors. These are individuals who will go out to their communities and work with our patients to increase awareness about genetic research and how important it is to be aware of the opportunities [for testing]. Several [of these individuals] are Latinas themselves whom I’m excited to engage in this work.
Domchek: We have two other things we’ve done at the Basser Center to take on the the fact that we don’t have providers that look like our patients. When you look at genetic counselors, almost none are individuals of color.
So this summer we had a program for college students, undergraduates, and underrepresented minorities to come to see what genetics is all about. We also were very fortunate that, with generous donors through the Basser Center, we have been able to fund an endowment so we can give scholarships for the genetic counseling program at Penn to underrepresented minorities. Because one of the challenges is that medical school is very expensive, but [many doctors] do earn a decent salary at the end. Genetic counseling school is also very expensive, and the salaries are not commensurate with physician salary. So it’s a very high bar if you’re going to incur debt that’s going to be hard to pay down. That is a huge barrier. We’re hopeful that this will diversify the workforce.
Lauren Puckett-Pope is a staff culture writer at ELLE, where she primarily covers film, television and books. She was previously an associate editor at ELLE.